Best Doctor for Peripheral Vascular Disease in Borivali
What is peripheral vascular disease?
Peripheral vascular disease (PVD), is a progressive circulation disorder characterized by the narrowing, blockage, or spasms in blood vessels.
Blood flows from the heart to every organ system in blood vessels known as arteries, while blood travels back to the heart in blood vessels known as veins.
PVD can affect any blood vessel outside of the heart, including arteries and veins, however arteries are more commonly affected, hence it is also known as a peripheral arterial disease (PAD).
Insufficient blood flow caused by PAD can impact various organs, but the condition predominantly affects the legs and feet.
What are the causes of peripheral vascular disease?
Peripheral artery disease is often caused by a buildup of fatty, cholesterol-containing deposits (plaques) on artery walls known as atherosclerosis. Plaque reduces the amount of blood flow to the limbs. It also decreases the oxygen and nutrients available to the tissue. As plaque builds up, your blood vessels get narrower and narrower, until they’re blocked. Blood clots may also form on the artery walls, further decreasing the inner size of the blood vessel and block off major arteries.
Less common causes of peripheral artery disease include:
- Blood vessel inflammation
- Injury to the arms or legs
- Changes in the muscles or ligaments
- Radiation exposure
- Infection
People with coronary artery disease (CAD) often also have PVD.
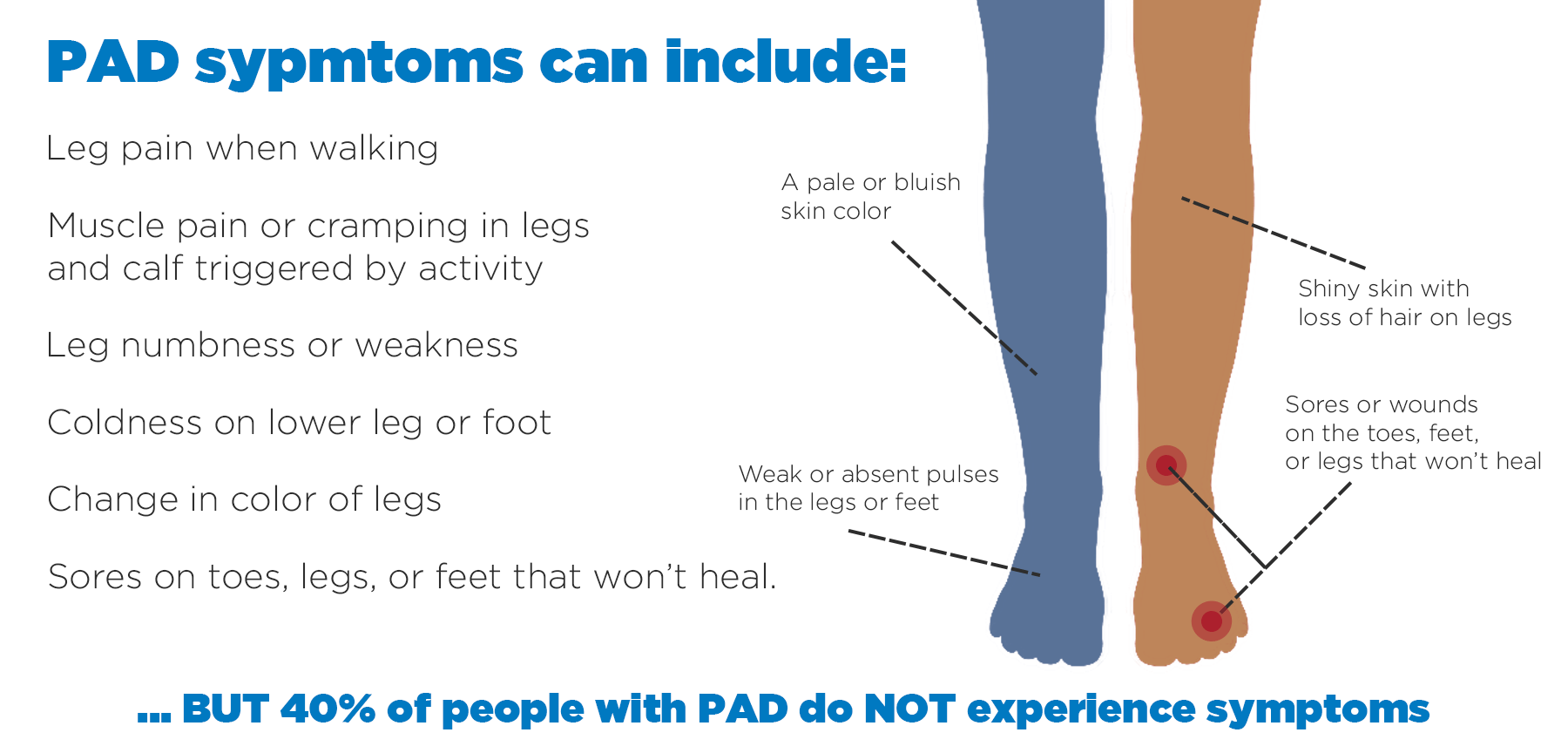
What are the symptoms of Peripheral arterial diseases?
Many people with PAD have no symptoms. However, some develop a painful ache in their legs when they walk, which usually disappears after a few minutes of rest. The medical term for this is “intermittent claudication”.
The pain can range from mild to severe and usually goes away after a few minutes when you rest your legs.
Both legs are often affected at the same time, although the pain may be worse in 1 leg.
Other symptoms of PAD can include:
- Hair loss on your legs and feet
- Numbness or weakness in the legs
- Brittle, slow-growing toenails
- Ulcers (open sores) on your feet and legs, which do not heal
- Changing skin colour on your legs, such as turning paler than usual or blue
- Shiny skin
- The muscles in your legs shrinking (wasting)
The symptoms of PAD often develop slowly, over time. If your symptoms develop quickly, or get suddenly worse, it could be a sign of a serious problem requiring immediate treatment.
Listen to your legs! If you’re experiencing any of these symptoms, it’s time to act. Schedule a consultation now to discuss and explore treatment options for Peripheral Arterial Disease Treatment in Borivali.
What are the risk factors for peripheral arterial disease ?
Smoking or having diabetes greatly increases the risk of developing peripheral artery disease.
Other risk factors include:
- Family history of peripheral artery disease, heart disease or stroke
- High blood pressure
- High cholesterol
- Increasing age, especially after 65 (or after 50 if you have risk factors for atherosclerosis)
- Obesity (a body mass index over 30)
- High levels of an amino acid called homocysteine, which increase the risk for coronary artery disease
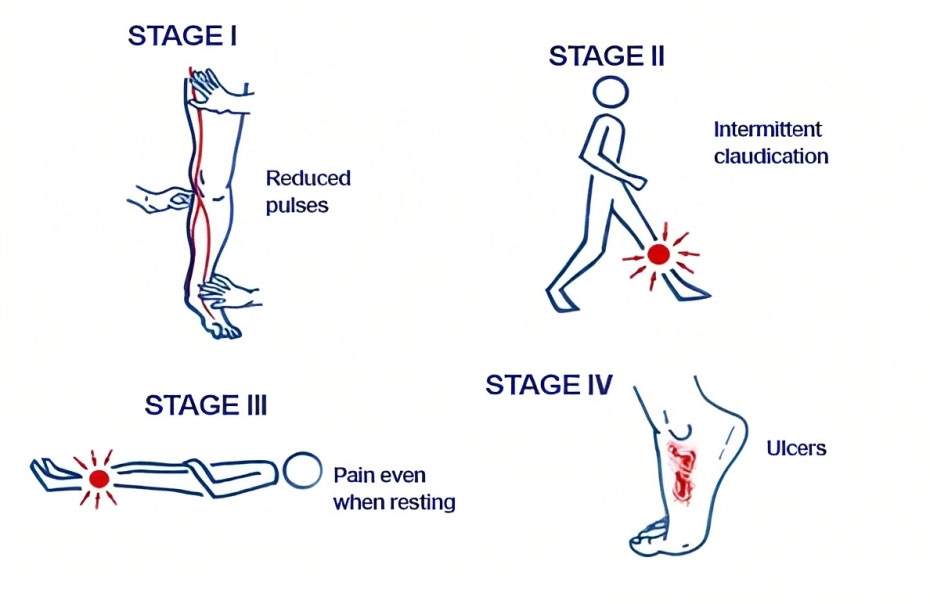
What are the stages of peripheral vascular disease?
Different classification systems can be used to assign a stage to your PAD. The Fontaine stages, which are simpler, are:
I: Asymptomatic (without symptoms).
IIa: Mild claudication (leg pain during exercise).
IIb: Moderate to severe claudication.
III: Ischemic rest pain (pain in your legs when you’re at rest).
IV: Ulcers or gangrene.
How to diagnose peripheral vascular diseases?
Medical history and physical examination: The doctor will ask about your symptoms, medical history, risk factors, and perform a physical examination to assess the signs of PVD, such as weak or absent pulses, coolness or pallor of the affected limbs, and signs of poor wound healing.
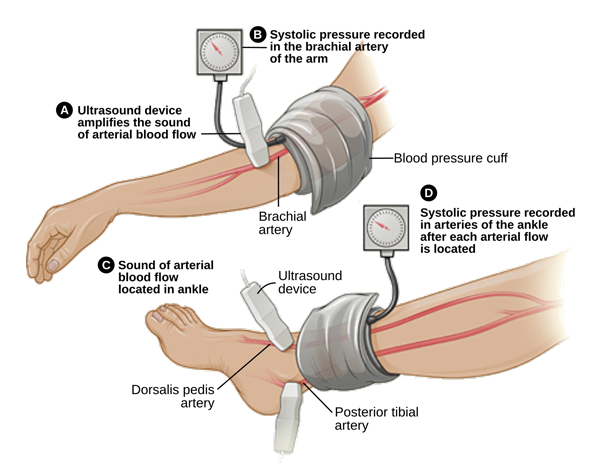
Ankle-brachial index (ABI):
This non-invasive test compares blood pressure measurements at the ankle and arm to assess the blood flow in your limbs. To determine the ABI, the systolic blood pressure(the top number of the blood pressure measurement) of the ankle is divided by the systolic blood pressure of the arm. A lower ABI value indicates reduced blood flow, indicating PAD.
Doppler ultrasound:
This test uses sound waves to evaluate blood flow in the arteries. It can detect any narrowing or blockages in the blood vessels and determine the extent of PVD.

Magnetic resonance angiography (MRA):
This imaging technique uses magnetic fields and radio waves to produce detailed images of blood vessels. MRA can help visualize the blood flow and detect any abnormalities or blockages.
Computed tomography angiography (CTA):
A non-invasive test, CTA uses X-ray and contrast dye to create detailed images of the blood vessels, providing detailed information about the extent and location of blockages in your legs. This is the most reliable and specific non-invasive method for diagnosis of PAD.

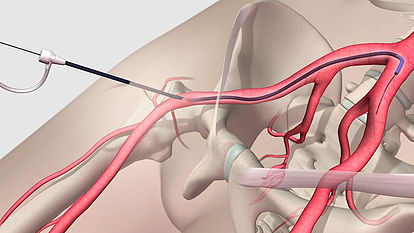
Angiography:
This is the gold standard method for the diagnosis of peripheral arterial disease. It is an invasive procedure, where a thin, flexible tube is inserted into an artery in the leg followed by injection of a contrast dye. This contrast dye makes arteries and veins visible on X-ray. It allows real-time evaluation of flow within blood vessels and helps identify any blockages or narrowing.
What are the symptoms of Peripheral arterial diseases?
- Non-healing wounds
- Increased risk of infection
- Tissue damage
- Gangrene
- Critical limb ischemia (CLI)
- Heart attack
- Stroke
How can peripheral arterial disease be treated ?
The goals of treatment for peripheral artery disease is:
- Manage symptoms, such as leg pain, blackening, or ulcer, so as to improve your quality of life.
- Improve artery health to reduce the risk of heart attack and stroke.
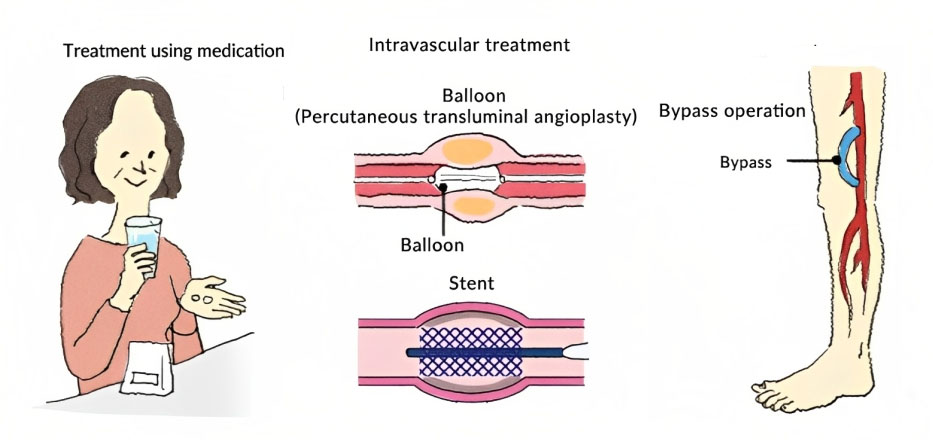
Depending on the severity of the peripheral arterial disease (PAD) and diagnostic testing results, medical treatment, minimally invasive endovascular treatment or surgical treatment option may be offered.
Lifestyle changes:
For mild PAD sufferers, lifestyle changes may be enough to slow or even halt the progression of your disease. Commonly prescribed lifestyle changes include:
- Stop smoking
- Exercise regularly
- Eat a healthy diet that’s low in fats and cholesterol
- Manage underlying conditions like diabetes or high blood pressure
Medications: PAD patients may receive medications to prevent blood clots(blood thinners), improve blood flow, and reduce pain from claudication. In addition, medications may be used to control your high cholesterol, high blood pressure, or diabetes.
If your leg pain is so severe that it prevents you from carrying out everyday activities, or if your symptoms have failed to respond to lifestyle changes and medical treatment, revascularization may be recommended.
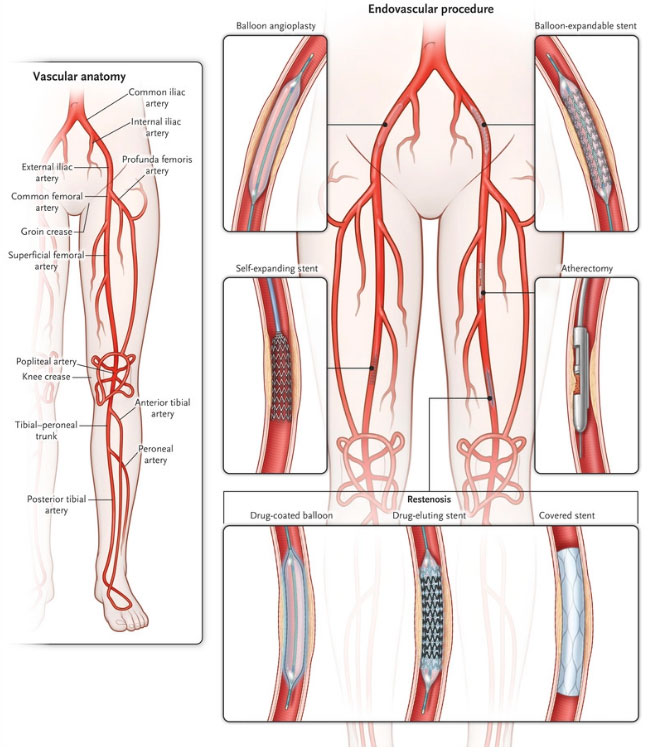
Endovascular (Interventional Radiology) treatment: Minimally invasive procedures such as angioplasty, stenting and thrombolysis may be offered to restore the flow in blocked arteries of your legs.
Surgical treatment: This involves inserting a graft bypass to move blood around the blocked or narrowed artery. The graft may be made from a vessel taken from another part of your body or using synthetic materials.
How does interventional radiologist treat peripheral arterial disease?
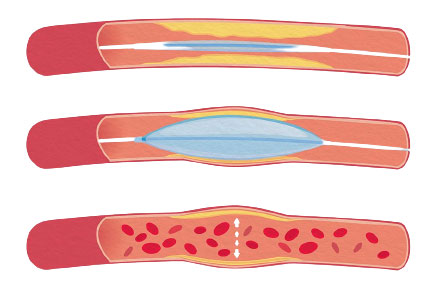
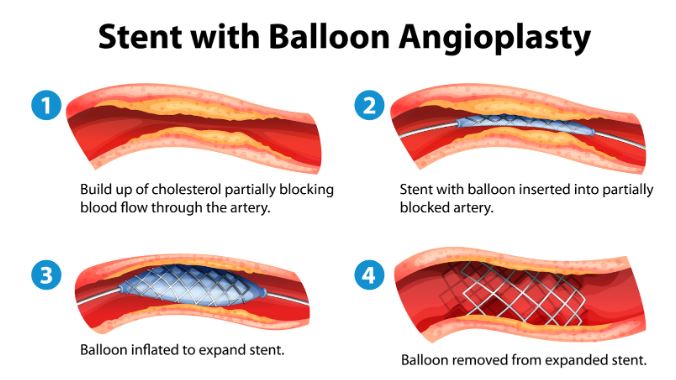
Angioplasty is a minimally invasive procedure performed under local anesthesia to open narrowed or blocked blood vessels that supply blood to your legs. It involves using a balloon-tipped catheter that is inserted into the affected artery. The balloon is then inflated, widening the artery and compressing the plaque, thereby restoring blood flow.
Angioplasty can be performed with plain balloons or drug-coated balloons to improve overall blood circulation.
Stenting is often used in conjugation with balloon angioplasty for the treatment of PVD. A stent, which is a small mesh tube, is placed in the treated artery during or after angioplasty. The stent acts as a scaffold, keeping the artery open and allowing for improved blood flow. Interventional radiologists carefully position and deploy the stent using specialized techniques. Stenting helps maintain the long-term effectiveness of the treatment by preventing the artery from narrowing again. It can provide lasting relief of symptoms and promote better circulation in the affected area.
Atherectomy is another minimally invasive procedure used to remove or break down plaque from the walls of blocked or narrowed arteries. Specialized tools, such as rotating blades or lasers, are employed to effectively remove the plaque and restore blood flow. Atherectomy serves as an alternative to traditional open surgery for treating PVD. By clearing the blockage and improving arterial function, atherectomy can provide symptomatic relief, enhance mobility, and improve overall vascular health.
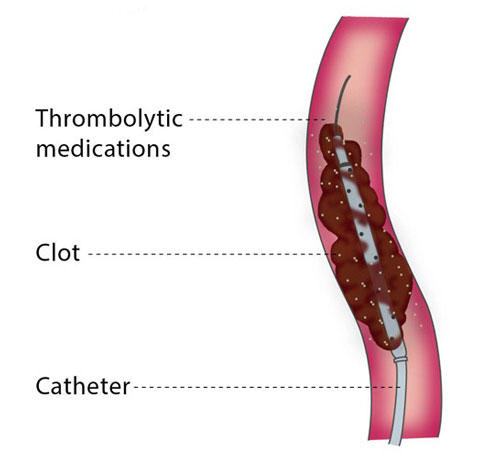
Thrombolysis is a treatment option for acute PVD cases caused by recent blood clots. During this procedure, we administer medication directly into the clot to dissolve it. The goal is to restore blood flow and alleviate the associated symptoms. Thrombolysis can be a life-saving intervention, particularly in cases of acute arterial occlusions.
Overview of all treatment options for PAD
What are the benefits and advantages of Endovascular treatments over surgery?
Minimally invasive: Endovascular procedures involve small incisions or punctures, reducing the need for large surgical incisions and minimizing trauma to surrounding tissues.
Lower risk of complications: The less invasive nature of endovascular treatments decreases the risk of complications such as infection, bleeding, and scarring.
Quicker recovery: Patients undergoing endovascular procedures often experience shorter hospital stays and faster recovery times compared to traditional surgery, allowing for a quicker return to daily activities.
Local anesthesia: Many endovascular procedures can be performed under local anesthesia, eliminating the need for general anesthesia and reducing associated risks.
Improved outcomes: Endovascular techniques have shown comparable or even superior outcomes to surgery in treating PAD, resulting in improved blood flow and symptom relief.
How to prevent peripheral arterial disease?
Quit smoking: Quitting smoking can significantly reduce the risk of developing PAD and slow down its progression if already diagnosed.
Exercise regularly: Engage in regular physical activity such as walking, running, cycling, or swimming. Exercise helps improve blood circulation, maintain a healthy weight, and reduce the risk of PVD.
Eat a healthy diet: Follow a balanced diet rich in fruits, vegetables, whole grains, lean proteins, and healthy fats. Limit your intake of saturated fats, cholesterol, and sodium.
Manage your blood pressure: Monitor and control your blood pressure through a combination of a healthy diet, regular exercise, weight management, and medication if prescribed by a healthcare professional.
Control your cholesterol levels: Maintain healthy cholesterol levels by consuming a low-fat and low-cholesterol diet, exercising regularly, and taking medications if prescribed.
Manage diabetes: Proper diabetes management can help prevent or slow down the progression of PAD.
Maintain a healthy weight: Aim for a healthy weight range by adopting a balanced diet and engaging in regular physical activity. Losing weight if overweight or obese can significantly reduce the risk of PAD.
Limit alcohol consumption: Excessive alcohol intake can contribute to the development and progression of PAD.
Take prescribed medications: If you have specific risk factors or medical conditions that increase the likelihood of developing PAD, such as high blood pressure or high cholesterol, take prescribed medications as directed by your doctor.
Regular check-ups: Visit your doctor regularly for routine check-ups, particularly if you have risk factors for PAD. Early detection and intervention can help prevent or manage the condition effectively.
Start your wellness journey today! Say goodbye to smoking, indulge in activities that bring you joy, eat wholesome meals, and team up with your Interventional Radiologist doctor for regular check-ins.
To book an appointment call on +91 90040 93090.